Printer Friendly
Provided
by:
The
National Osteonecrosis Foundation
and
The Center for Osteonecrosis Research and Education
OSTEONECROSIS
INTRODUCTION
Osteonecrosis
(ON) affects approximately 20,000 new patients per year in the
United States. Although any age group may develop ON, most patients
are between 20 and 50 years old, with the average age in the late
30's. The diagnosis of ON does not affect life expectancy, and
for this reason several hundred thousand patients are living with
this disease in the U.S. alone.
What
is osteonecrosis? First, you should understand that bone is a
living tissue with living cells and a blood supply. Osteonecrosis
means death of bone which can occur from the loss of the blood
supply or by some other means (see ‘What Causes Osteonecrosis?’).
It has been known by a number of other names including ischemic
necrosis of bone, aseptic necrosis or avascular necrosis (AVN).
AVN has been quite popular in its use because it is shorter to
say and write. More recently the term ON (osteonecrosis) has been
adopted.
In
the following sections, a review of the factors that play a role
in your individual treatment and results of those treatments are
discussed. It is important to understand that each patient is
unique. Differences in the amount of bone involvement, other diseases
that you may have, your level of activity, and other factors are
extremely important in determining the appropriate treatment for
each individual patient. None of the information presented here
is intended to take the place of the individual patient-physician
encounter. Rather, this brochure is designed to help you understand
more about the disease and will assist you in discussing specific
treatment options with your physician.
Who’s
at Risk?
If
a person is completely healthy, the risk of getting osteonecrosis
is quite small, probably less than one in 100,000. Another way
to understand this is that most of the people who get ON probably
have an underlying health problem. Most patients are between 20
and 50 years old with an average age of 38. Patients over the
age of 50 are likely to have developed ON either by a fracture
of the hip or more rarely in association with disease of the major
blood vessels to the lower leg.
Legg-Calve-Perthes
Disease
Children,
ranging in age from 2 to early teenage years, get a form of osteonecrosis
called Legg-Calve-Perthes disease (Perthes for short) after the
three doctors who first described it. Treatment for Perthes is
completely different than for adult ON. A pamphlet describing
this disease is available from the National
Osteonecrosis Foundation.
What
Causes Osteonecrosis?
There
are two major forms of ON, post-traumatic and non-traumatic. Examples
of post-traumatic ON, a common cause of ON, include displaced
fractures or dislocations. Minor trauma is not believed to cause
ON. Even major injury does not often result in ON. Certain kinds
of fracture, where the blood vessels to part of the bone have
been physically damaged, may result in ON.
Non-traumatic
ON occurs when their is no history of trauma. Scientists have
identified a number of risk factors that may be associated with
non-traumatic ON. We do not know how these risk factors may lead
to the development of the disease. There are many different ideas
(also called hypotheses). But these ideas have not been proven.
There are some cases of osteonecrosis that occur in patients that
are otherwise completely healthy with no detectable risk factors.
This catagory is called "idiopathic", a word meaning
"of unknown cause".
What
are the Risk Factors?
One
of the most common causes of osteonecrosis of the hip and of other
joints is a displaced fracture or a dislocation. However, this
brochure focuses on non-traumatic osteonecrosis. The risk factors
for osteonecrosis can be separated into two catagories: definite
and probable. The most common risk factor is a history of high
dose steroid treatment for some medical condition (e.g., Lupus).
Low dose steroids (cortisone, prednisone, etc.) commonly used
for bee stings, poison ivy and acute allergies are not thought
to cause osteonecrosis. The next most common associated condition
is a history of high alcohol use. The greater the alcohol consumption,
the higher the risk of osteonecrosis.
| CAUSES
OF OSTEONECROSIS |
| DEFINITE
|
PROBABLE
|
| |
- Corticosteroids,
High Dosages
|
|
| |
|
|
- Caisson
Disease
(Deep Sea Divers) |
|
|
| |
- Connective
Tissue Disease
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
First
Symptoms
Unfortunately
many patients with ON have had the disease for quite some time
before symptoms are present. The initial symptoms are usually
felt during activity and include pain or aching in the affected
joint. Symptoms usually begin slowly and may initially be sporadic.
Sometimes, the pain may begin quite suddenly. As the disease progresses,
the pain increases and is associated with stiffness and loss of
motion of the involved joint. Limping becomes common. The hip
is the most common joint affected, and the pain is usually felt
in the groin.
Progression
of the Disease
In
the earliest stage of the disease, x-rays appear normal and the
diagnosis is made using MRI. Once it can be seen on x-ray, it
is not actually the dead bone that can be seen but the healing
response of the living bone to the area of necrosis. The advanced
stages of ON begin when the dead bone starts to fail mechanically
through a process of microfractures of the bone. Eventually, this
will result in damage to the other side of the joint, requiring
major joint reconstruction.
| |
These
x-rays of the hip show the different stages of the disease.
At first (stage I), there are no detectable changes on x-ray
(fig A). In stage II, there are some changes but the surface
is still intact (fig B). As the disease progresses, the surace
begins to collapse (fig C) until, finally, the integrity of
the joint is destroyed (fig D). |
In
the more advanced stages of the disease and/or when more of the
joint is damaged, it is less likely that the natural joint can
be preserved. Fortunately, joint replacement procedures today
are highly successful, even in the relatively young patients affected
by ON. It is always the physicians desire to preserve the normal
joint whenever possible. Unfortunately many patients do not visit
the doctor until their joint has an advanced stage of the disease.
Extent
of Disease
The
femoral head (the ball part of the hip) is the most frequent bone
involved and will be used for this discussion. It is rare for
the entire weight-bearing surface of the femoral head to be involved.
However if more than half of the surface is involved, treatments
designed to preserve the femoral head have a much lower chance
of success.
| MRI's
of Femoral Heads
diagnosed with Osteonecrosis |
| |
|
| Small
Lesion |
Large
Lesion |
How
Is Osteonecrosis Diagnosed?
The
first, and most important, thing that a physician can do is to
perform a thorough physical examination and to ask questions about
your medical history. Once there is a suspicion of osteonecrosis,
your physician will likely obtain one or more of the following
tests:
- X-ray
- Magnetic
Resonance Imaging (MRI)
- Bone Scan
- Computed
Tomography (CT)
- Biopsy
The
principle diagnostic tool is the x-ray. By the time that most
patients have significant symptoms, the disease is advanced enough
to be seen on standard x-rays. In most cases the x-ray will show
the area of bone that is involved. However, the very earliest
stages of ON cannot be seen on a regular x-ray. A widely used
tool is called an MRI. [This test does not involve x-ray radiation.]
These special images are able to detect tissue changes that are
not seen on a plain x-ray. Occasionally, your doctor may order
a CT scan, which is a special series of x-rays interpreted by
the computer to show the three dimensional structure of the bone.
Any of these tests will help the doctor to determine how advanced
the disease is in your case.
TREATMENT
Introduction
Before
entering into a description of some of the treatments available
for ON, it is important to understand the concept of risk/benefit
ratio. Any surgical procedure has a certain element of risk involved.
Even no treatment at all has the risk that the disease will progress,
so doing nothing is not risk free. Some procedures may have a
lower likelihood of success but have very little risk. Other procedures
may have a higher degree of success, but also have a higher degree
of risk. The physician must work with the patient in assessing
all the factors that evaluate both risk and benefit for the patient
in their particular circumstance. What is right for one patient
may be absolutely wrong for another. This is particularly true
for ON because each patient presents with a unique set of factors
(age, associated disease, specific joint(s) involved, extent and
progression of disease). Any treatment needs to be determined
between you and your treating physician. Ask questions, get answers!
Non-Surgical
Treatment
Protected
weight bearing Canes,
crutches or a walker are useful in alleviating the pain
associated with ON. They can also be useful in protecting the
joint between the time of diagnosis and scheduling of elective
surgery. Limiting weight bearing may also play a role in limiting
progression while associated medical conditions are managed. However,
protected weight bearing alone is never an adequate treatment
for ON nor will it result in cure of the condition, no matter
how long it is maintained. Rarely, an associated medical condition
may result in a patient not being able to have surgery. In this
case, protected weight bearing may be recommended for pain management.
Pharmaceutical
Treatment for Osteonecrosis
There
are no established pharmaceuticals (drugs) for the prevention
or treatment of osteonecrosis. In order to treat the disease,
we must first understand how the disease develops. In spite of
considerable effort by researchers, we still do not know for sure
what causes some forms of osteonecrosis (that is, the forms that
are not a result of a fracture or radiation). We’ve identified
several risk factors, but it is not known what effect eliminating
or treating the risk factors has on the disease once the disease
has begun. However, this is not meant to be a pessimistic outlook
for the pharmaceutical treatment of osteonecrosis. There are several
studies that are being undertaken to evaluate the potential of
pharmaceutical treatment. This article will summarize their findings
to date.
There
are several levels of evidence that can be used to support a position
by the medical community. They range from the treatment of one
patient (a case report) to comprehensive studies evaluating large
numbers of patients. Most of the studies concerning the pharmaceutical
treatment of osteonecrosis fall somewhere in between – with
many being a report of a series of patients treated with a medication
with no control group receiving a placebo. It is important to
understand this so that you can place the significance of these
reports in their proper context.
Lipid
Lowering Agents
Two hypotheses concerning osteonecrosis relate to lipids (fats).
One hypothesis proposes that there is an increase in the number
of fat cells (lipocytes) in the bone marrow of the diseased joint.
Another hypothesis is that there is an increase in the amount
of fat contained within cells that eventually causes the cell
to malfunction or die. With this in mind, scientists have investigated
whether lipid-clearing agents can be used to prevent the development
of osteonecrosis1,2,3. In a clinical study of 284 patients taking
high dose corticosteroids – the type of steroid used to
treat inflammation, a lower incidence of osteonecrosis (1%) was
found than is usually reported for this patient population (3-20%)3.
Further studies are needed to confirm or disprove these findings.
Anticoagulants
There is increasing evidence that there are abnormal levels of
specific factors involved in the coagulation/blood clotting system
in some patients with osteonecrosis4,5. One study evaluated the
use of Stanozolol, an anabolic steroid, in 5 patients6. They had
variable results with several patients having relief of pain yet
progression of the disease as observed by x-rays. In a separate
study, twenty-eight patients (35 hips) were treated for 12 weeks
with Enoxaparin, a drug used to prevent clotting or prevent existing
clots from getting larger (an anticoagulant) 7. After two years,
most of the hips had not progressed past the early stage of the
disease (Ficat Stage I or II) and most (31/35) did not require
surgery. Further studies are needed to confirm or disprove these
findings.
Hypertensive
Medications
Hypertensive medications are drugs used to treat high blood pressure.
Several studies have shown that osteonecrosis is associated with
an increase in the pressure within the affected bone. One surgical
treatment for this is core decompression. It is believed that
a core biopsy or biopsies in the diseased bone relieves the pressure
and thereby relieves the pain. Another approach to this would
be to treat the patient with blood pressure lowering medications.
In one study, seventeen patients with early stage osteonecrosis
underwent treatment with ilioprost, a vasodilator – a drug
used to reduce high blood pressure8. At one year, function and
pain levels improved for these patients. The average clinical
assessment scores were significantly improved following treatment.
They also found that the amount of bone edema (extra fluid) present
in the bone was significantly less. Similar results were found
for another drug, Nifedipine9. Further studies are needed to confirm
or disprove these findings.
Bisphosphonates
Bisphosphonates are a class of drugs that have been used to treat
osteoporosis – a disease that is characterized by a low
bone mass. Recently, in an effort to reduce bone loss, one bisphosphonate
- alendronate has been evaluated in 60 patients diagnosed with
osteonecrosis of the hip10. All patients had symptomatic improvement
at one year. Although the follow-up time ranged from three months
to five years, only six patients (ten hips) progressed to the
point of needing surgery. It is important to note that these patients
were also instructed to avoid bearing weight on their affected
hip. Recently, concern has been raised relating to a possible
association between bisphosphonate therapy and an increased incidence
of osteonecrosis of the jaw11,12. Further study is needed to clarify
this possible complication.
Drug
Studies
You do not need to be in a drug study to receive pharmaceutical
treatment for osteonecrosis. These medications are not experimental
and can be prescribed by a physician. However, whether they will
be prescribed for you is dependent on the physicians experience
and your individual circumstance (the size of the affect area,
how far along the disease has progressed, for example). As we
have emphasized, all of these treatments must be evaluated more
thoroughly before the medical community will accept them as standard
treatment.
References
- Cui et
al. CORR 1997; 344: 8-19.
- Wang et
al.CORR 2000; 370: 295-310.
- Pritchett
JW CORR 2001; 386:173-8.
- Glueck
et al. Clin Orthop Relat Res. 1997 Jan;(334):43-56.
- Jones
et al. J Rheumatol. 2003 Apr;30(4):783-91.
- Glueck,
Freiberg, Wang Curr Hematol Rep 2003; 2:417-422.
- Glueck
CJ, Freiberg RA, Sieve L, Wang P. Enoxaparin prevents progression
of stages I and II osteonecrosis of the hip. Clin Orthop Relat
Res. 2005 Jun;(435):164-70.
- Disch
et al. J Bone Joint Surg Br. 2005 Apr;87(4):560-4.
- Laroche
et al. Rev Rhum Mal Osteoartic. 1990 Oct;57(9):669-70.
- Agarwala
Rheumatology 2005 Mar 44(3): 352-9
- Maerevoet
NEJM 2005 Jul 7; 353(1): 99-102
- Ruggiero
J Oral Maxillofac Surg 2004 May 62(5): 527-34
Surgical
Treatment
Core
Decompression
This
is a surgical procedure that involves taking a plug of bone out
of the involved area. It is applicable for mild to moderate degree
of involvement that has not yet progressed to collapse. Because
this involves creating a 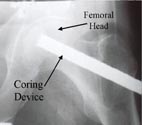 hole
in the bone, six weeks of protected weight bearing is necessary
to avoid fracture through the hole. Pain relief from this procedure
has been excellent, but it has not been as effective at delaying
the progression of the disease in the long term. In centers that
do this procedure frequently, most studies have reported good
results in the appropriate cases. However, there is some controversy
about this procedure with a few studies that have been reported
showing generally poor results.
hole
in the bone, six weeks of protected weight bearing is necessary
to avoid fracture through the hole. Pain relief from this procedure
has been excellent, but it has not been as effective at delaying
the progression of the disease in the long term. In centers that
do this procedure frequently, most studies have reported good
results in the appropriate cases. However, there is some controversy
about this procedure with a few studies that have been reported
showing generally poor results.
Bone
Grafting When a section
of the bone has died, as is the case in ON, it doesn’t spontaneously
heal. One approach to this problem is to surgically remove the
dead bone and fill the empty space with bone graft that is either
taken from the patient or from the bone bank. The success of this
approach depends upon the quantity of bone that has died.
Vascularized
Bone Grafting
Regular
bone graft, whether from the bone bank or from the patient, is
itself dead bone. It serves as a scaffold for the body to build
new bone around, but the body also has to grow a new blood supply.
For this procedure, a bone with its blood vessels is taken from
the patient and hooked up to blood vessels near the hip. The dead
bone is removed from the femoral head and replaced with the grafted
bone that carries with it its own blood supply. The advantage
of this approach is that the body doesn't have to rebuild a new
blood supply and the bone graft keeps its physical and mechanical
properties. This is most appropriate prior to the collapse of
the joint, but is sometimes used in cases with early (limited)
collapse.
Healing
and complete filling of the defect still has to take place, during
which time crutches or a walker has to be used. The disadvantage
of this procedure is that a substantial piece of bone has to be
taken from the lower leg (the fibula, the smaller bone of the
lower leg below the knee). Some patients may develop pain in the
area from which the bone graft is taken. The operation also takes
several hours and requires a team experienced in these techniques.
The patient is also required to be on crutches for several months.
If both hips are involved, it may be necessary to delay treating
one hip for quite some time during which period the femoral head
may undergo collapse.
Osteotomy
(Cutting the Bone) Usually
the location of the ON is in the area of the bone that bears weight.
In some cases the bone can be cut below the area of involvement
and rotated or turned so that another portion of the bone, that
is not involved in the ON, can become the new weight-bearing area.
These operations are not very common anymore, but may apply to
special cases with smaller lesions.
Femoral
Head Resurfacing [FHR]
Initially
only the femoral head is involved, not the socket of the hip joint.
FHR involves implanting a metal hemisphere over the femoral head,
which exactly matches the size of the original femoral head. This
is similar to capping a tooth when the root is still good, as
opposed to pulling the tooth and putting in a false tooth. It
is known that over a period of many years, the metal head will
gradually wear out the socket and will need to be converted to
a total hip replacement. This procedure is designed to "buy time"
for the younger individual 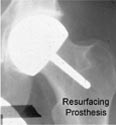 whose
extent of disease or degree of progression is such that one of
the preservative procedures listed above cannot be performed.
Most patients with ON are under 50. It is generally believed that
total hip replacement (THR) today will not last the 30+ years
most of these patients will require. Therefore, it is possible
that at least two procedures will be necessary for the treatment
of this disease during a patient’s lifetime. If the 2 procedures
are a femoral head resurfacing followed later by a primary total
hip replacement, this is preferable to a primary THR followed
by a revision THR. However, although the early results have been
favorable, FHR is still a relatively new procedure which is currently
being evaluated.
whose
extent of disease or degree of progression is such that one of
the preservative procedures listed above cannot be performed.
Most patients with ON are under 50. It is generally believed that
total hip replacement (THR) today will not last the 30+ years
most of these patients will require. Therefore, it is possible
that at least two procedures will be necessary for the treatment
of this disease during a patient’s lifetime. If the 2 procedures
are a femoral head resurfacing followed later by a primary total
hip replacement, this is preferable to a primary THR followed
by a revision THR. However, although the early results have been
favorable, FHR is still a relatively new procedure which is currently
being evaluated.
Femoral
Head Replacement
This
is basically half a total hip replacement. All comments about
femoral head resurfacing apply to femoral head replacement. However,
because a femoral head replacement also puts a stem inside the
femoral bone (the femoral shaft) it is a little more extensive
than the resurfacing procedure. If it needs to be revised, it
is a little more difficult to convert to a total hip replacement
than the resurfacing procedure. There is also no evidence that
a femoral head replacement is more successful than a femoral head
resurfacing.
Metal-on-Metal
Resurfacing The
original concept of replacing the surface of the femoral head
with metal and the acetabulum with a plastic liner had a high
failure rate due to failure on the acetabular side. The concept
has reappeared with a metal liner on the socket side. Experience
is limited but the procedure shows promise.
Total
Hip Replacement [THR]
When
the ON is advanced to the point that there is involvement of the
socket as well, then the only thing that will be effective is
either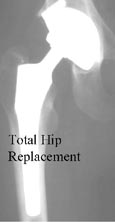 a hip fusion (making the hip completely stiff) or a total hip
replacement (THR). THR is one of the most successful surgical
procedures ever devised. Success rates are usually above 95%!
The problem with total hip replacements for patients with ON is
that it is not uncommon for the patient to have a life expectancy
of more than 40 or even 50 years. With current technology we don't
think that it is likely that a THR will last that long. For this
reason, many physicians will want to try some procedure to put
off THR for a few years even when it is known that that procedure
will not in itself be successful forever. If your disease is advanced,
and/or extensive, then THR may be the only thing that makes sense.
Work is currently in progress to develop and evaluate newer total
hip replacements, such as ceramic-on-ceramic devices, which may
be much more durable than present components, and which theoretically
might last a lifetime even in younger patients with ON.
a hip fusion (making the hip completely stiff) or a total hip
replacement (THR). THR is one of the most successful surgical
procedures ever devised. Success rates are usually above 95%!
The problem with total hip replacements for patients with ON is
that it is not uncommon for the patient to have a life expectancy
of more than 40 or even 50 years. With current technology we don't
think that it is likely that a THR will last that long. For this
reason, many physicians will want to try some procedure to put
off THR for a few years even when it is known that that procedure
will not in itself be successful forever. If your disease is advanced,
and/or extensive, then THR may be the only thing that makes sense.
Work is currently in progress to develop and evaluate newer total
hip replacements, such as ceramic-on-ceramic devices, which may
be much more durable than present components, and which theoretically
might last a lifetime even in younger patients with ON.
Osteonecrosis
of the knee and shoulder and ankle
Ninety
per cent of patients afflicted by osteonecrosis have osteonecrosis
at the hip. However osteonecrosis also can attack the knee, shoulder
and ankle in that order frequency. Moreover, patients who have
osteonecrosis at the hip are more likely to have another joint
involved. However, any of these other joints can be involved independently.
About 3% of patients with osteonecrosis will have more than two
joints involved. The most common combination is hip and knee.
It is uncommon for the shoulder or ankle to be involved as an
isolated joint. Much of what has been written earlier about osteonecrosis
of the hip also applies to these other joints. The classification
systems are essentially the same, and the progression of the disease
is similar, passing from x-ray negative, to x-ray positive without
collapse, too early collapse and finally to extensive joint destruction.
These other joints also may experience small or large lesions
with the same significance as for the hip. The larger the lesion,
the more likely it is to collapse. The further the progression,
the less likely that the joint can be preserved. There are some
differences with each of the individual joints in both treatment
and consequences of osteonecrosis which are based partly on the
function of those joints, partly on the anatomy, and partly on
the success of joint replacement which is the ultimate treatment
for advanced disease. This section will detail each of the joints
and their peculiarity.
Osteonecrosis
of the knee -- the knee is the second most common
joint to be affected by osteonecrosis. Although the numbers are
difficult to determine with any degree of accuracy, in our experience
we see about one case of osteonecrosis of the knee for every 10
cases of the hip. Although some of these patients will have knee
involvement as an isolated joint , most patients with osteonecrosis
of the knee will have osteonecrosis somewhere else. The knee is
a very complex joint and can really be divided into three compartments;
the medial compartment which is the inside of the knee between
the femur bone and the tibia or shinbone, the lateral compartment
which is the outside of the day the, and the patellofemoral compartment
(kneecap). The most common involvement is the distal femur or
the thigh bone portion of the knee. It is not uncommon for the
tibia or shinbone also to be involved, but it is unusual for the
patella (kneecap) to be involved.
In
the hip, if the lesion is large enough, progression to collapse
is almost certain. There are some small lesions, usually asymptomatic,
that do not collapse. This is not necessarily the case in the
knee. The natural history of osteonecrosis of the knee is less
certain than it is for the hip. In general we do not treat asymptomatic
osteonecrosis of the knee, i.e. osteonecrosis that is picked up
by MRI but for which the patient has no symptoms. If the patient
has symptoms, and the lesion has not collapsed, we have performed
and reported on core decompression with good success. Core decompression
usually results in immediate relief of symptoms. However, because
the natural history and natural progression of osteonecrosis of
the knee is less predictable, it is not certain that the core
decompression alters the natural history. We have had patients
with osteonecrosis and knee pain who have been treated with core
decompression and continued to have pain relief for up to 20 years.
Once
the osteonecrosis has progressed to collapse, the only treatment
is total knee replacement. In general, we do not recommend partial
knee replacement, because non-replaced areas of bone can progress,
leading to the need for revision or conversion of the partial
knee replacement to a total knee replacement. We have not yet
seen a patient whose osteonecrosis was so advanced or so extensive
that a total replacement could not be done.
Shoulder
-- osteonecrosis of the shoulder has an even more variable natural
history than the knee. The area of the involvement of the humeral
head (shoulder) is that area of the head which is in contact with
the socket when the elbow is held at about 40° of flexion
and 20° away from the body. It is possible to effectively
use one's hands with the elbows held at the side, and therefore
avoid contact of the humeral head with the socket in the area
to involvement with osteonecrosis. Therefore unless the lesion
is very large, or collapse is extensive, most patients will benefit
from core decompression. Although shoulder replacement is done,
the success rate is not as great as for the hip and knee, and
the results may not be as long-lasting. Therefore if a conservative
procedure like core decompression can grant the patient relief
of symptoms and delay the need for shoulder replacement, that
conservative procedure is justified. We have had good results
from core decompression even in those patients with early collapse.
This is not the case with early collapse of the hip, for which
core decompression should not be done except in unusual cases.
Ankle
-- the ankle bone (talus) is fortunately not involved with osteonecrosis
very often. It represents a real problem for the orthopedic surgeon
(and the patient). Historically ankle replacements have not been
very successful. Ankle fusion can be performed with extensive
bone grafting. However, when the ankle bone is involved with osteonecrosis,
because the bone is dead, ankle fusion is also not very successful.
We have had some limited success with core decompression and would
recommend it as a trial, mostly because nothing else works very
well. An exterior ankle brace may be necessary.
Can
It Be Prevented?
At
present, there is no known prevention. However, it is reasonable
to believe that if some of the risk factors are treated or eliminated,
you would decrease your risk for getting the disease. For this
reason, steroids should only be taken as necessary and alcohol
consumption should always be in moderation. Some experimental
drug protocols are being evaluated which may have a place in treatment
or prevention in the future.
Early
Recognition and Intervention
An
important message has been learned over the past few years in
the treatment of osteonecrosis. Early diagnosis and early intervention
provides the best opportunity for alleviating the collapse of
the joint surface and delaying the need for hip replacement surgery.
The only other treatment option is hip arthrodesis - surgical
fusion. Since this condition commonly occurs in both hips, it’s
important that both hips be thoroughly assessed at each evaluation.
Furthermore, if osteonecrosis is first diagnosed in a joint other
than the hip, the hip should also be evaluated.
THE
FUTURE
Currently,
there are several studies being conducted to evaluate drugs that
may lead to the prevention of this disease. The effectiveness
of these drugs has not been proven in scientifically controlled
studies in large numbers of patients. But they do offer hope for
the future.
Other
treatments are being evaluated to improve the results of the current
surgical treatments. Bone graft substitutes and electrical stimulation
are being studied in select centers throughout the country.
The
future is dependent on a better understanding of why some people
get the disease and some do not even when they have the same underlying
conditions (steroids, alcohol, etc.) Because the disease does
not affect large numbers and because most physicians do not see
a lot of patients with osteonecrosis, it is important that an
organization like the National Osteonecrosis
Foundation brings together
patients, their families, and physicians to promote increased
awareness of this disease and to support large scale research
efforts.
The
National Osteonecrosis Foundation
The
National Osteonecrosis Foundation is made up of a group of patients,
their families, physicians, and other caring individulas who are
interested in finding a cure for osteonecrosis. It is the mission
of this foundation to provide support for medical research and
for the education of patients, physicians, and other health professionals.
If you are interested in more information, please contact us:
The
National Osteonecrosis Foundation, Inc.
P.O. Box 518
Jarrettsville, MD 21084
PHONE: (443) 248-4889
Websites:
NONF
Website
http://www.osteonecrosis.org
Support
Group for Patients with ON
http://osteonecrosisavnsupport.org/index.html
Support
Group for Patients with Perthes
http://maxpages.com/lpsupportgroup
Home

